TTM2: Dankiewicz J, Cronberg T, Lilja G, et al. Hypothermia versus normothermia after out-of-hospital cardiac arrest. N Engl J Med. 2021;384:2283-2294. https://www.nejm.org/doi/10.1056/NEJMoa2100591
TL;DR
- Cooling comatose patients to 33°C after out of hospital cardiac arrest (OHCA) did NOT improve survival at 6 month compared to simply maintaining normothermia (<37.8°C)
- There was also NO difference in survival with severe neurological disability, quality of life, but there was a higher risk of arrhythmias in the hypothermia treated patients.
- The TTM2 trial is a well-designed trial that is the highest level of evidence to date. Current guidelines are based on previous studies with significant limitations.
- With no benefit of survival and risks, (ie. more paralytics and arrhythmias) cooling may not be as helpful as originally thought.
- Actively avoiding fevers using a temperature regulating device is still advisable.
- Focus on delivering excellent comprehensive post-arrest care.
Background:
- Animal studies and early clinical trials in humans suggested a benefit to hypothermia over normothermia after cardiac arrest. (Minimize reperfusion injury, makes sense to me)
- The HACA trial (2002) found targeted hypothermia of 33°C was associated with improved survival and neurological outcomes in patients with cardiac arrest and a shockable rhythm. (14% ARR in mortality! Sign me up! Don’t mind the limitations, we have got to be on to something!)
- A 2012 Cochrane review suggested that mild hypothermia likely improves survival and neurologic outcome after cardiac arrest. (Look at us, we are doing good things!)
- The TTM trial (2013) enrolled patients with both shockable and non-shockable rhythms found no differences in survival or neurologic outcomes between hypothermia (33°C) and normothermia (36°C) groups. (Cool, cool, cool. Aim for cool but not frozen – easier for us, better for them!)
- The HYPERION study (2019) compared 33°C to 37°C in patients with non-shockable rhythms finding favourable outcomes in the hypothermia group. (Hmmm, but how convincing? Let’s keep calm and cool-on)
- Initiating therapeutic hypothermia in the ED for post arrest patients is resource heavy and time intensive, and hypothermia itself poses some clinical risks for the patient.
Clinical Question:
- In adult patients with coma following out-of-hospital cardiac arrest, is targeted hypothermia at 33 °C followed by controlled rewarming associated with a lower mortality rate than targeted normothermia with early fever treatment?
Design: Prospective, randomized superiority trial. International, multicenter trial.
Patients: 1900 patients who were admitted after OHCA due to a primary cardiac or unknown cause, 1861 included in intention to treat analysis
Inclusion:
- Adults >18
- OHCA presumed cardiac or unknown cause
- Unconscious, not able to obey verbal commands, no verbal response to pain
- Sustained (20min) ROSC
- Eligible for ICU without restrictions or limitations
- Inclusion within 180min of ROSC
Exclusion:
- Unwitnessed cardiac arrest with an initial rhythm of asystole
- Temp of <30’C upon admission
- Requiring ECMO prior to ROSC
- Obvious or suspected pregnancy
- Intracranial bleeding
- Severe COPD requiring long-term home oxygen therapy
Intervention:
- Patients were randomized in a 1:1 ratio into one of two groups for an intervention period of 40 hours.
- 1) Hypothermia/intervention group: 925 patients, rapid target hypothermia via cold fluids and surface/intravascular cooling devices (cooling to 33°C x 28hr), followed by controlled rewarming to 37°C by changing 0.33°C per hour x 12 hours, then normothermia out to 72hr
- 2) Normothermia/control group:
925 patients, targeted normothermia with early fever treatment for patients in whom fever reached a threshold of 37.8°C (surface or intrasvascular cooling devices to aggressively maintain temperature of 37.5°C). This was maintained for 72hours in patients who remained sedated or comatose.
Outcome:
1) Primary: death from any cause at 6 months.
2) Secondary: poor functional outcome (score 4-6 on modified Rankin scale) at 6 months, hospital-free survival, health-related quality of life, survival in a time-to-death analysis, any of the following adverse events (arrhythmia, bleeding, skin complications, pneumonia, sepsis).
- Clinicians were non-blinded due to challenges blinding body temperature, however the assessors of clinical prognosis, participants, outcome assessors, statisticians and data managers were all blinded.
- Outcomes were assessed at 30 days, 180 days, and (ongoing) 24 months.
Results:
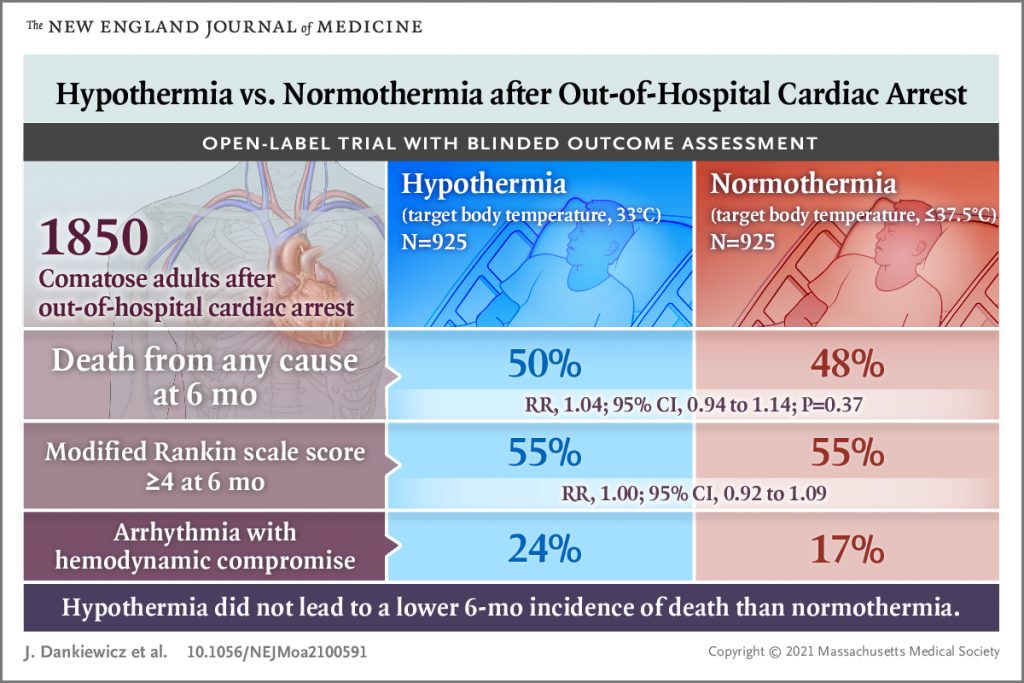
- There was no statistically significant different in the primary outcome: death from any cause at 6-months (hypothermia: 465/925, normothermia 446/925, RR 1.04, p=0.37)
- The only secondary outcome to be statistically significant at <0.001 was arrhythmia causing hemodynamic compromise. (hypothermia 24%, normothermia 17%, RR 1.45, 95% CI 1.21-1.75)
- The hypothermia group required more paralytics and longer duration of mechanical ventilation than the normothermia group
Limitations:
- Unclear if it can be applied to in hospital cardiac arrest
- Predominance of males in both groups (only ~20% females)
- There was no third group to answer the question as to whether temperature management is better than no temperature management.
- External validity is questionable is that 75% of patients had a shockable rhythm, 90% had bystander CPR, a cohort of patients we do not often see.
Strengths:
- Very thoughtful methodology, well organized
- Clear separation in temperatures between the two groups
- Large sample size (larger than combined enrolment of earlier trials) leading to less chance of random error in outcomes
- Large sample size and international, multi-centered trial helps external validity
- Low risk of bias in nature of primary outcome and assessors were blinded
- Physician performing neurological assessment at 96 hours for those patients who stayed in ICU was blinded
- Nearly complete follow-up with 94% retention at 6 months
Thoughts:
- Unique group captured: witnessed arrest, 90% had bystander CPR, and roughly half survived at 6 months.
- Perhaps with such quick bystander CPR and a shockable rhythm, the overall ischemic neurological burden was less.
- The care delivered to these patients is the pinnacle of ICU comprehensive post arrest care, independent of the temperature selected.
- At the minimum this trial highlights the importance of bystander CPR, efficient pre-hospital care, rigorous post-arrest critical care, as well as the importance of minimizing premature withdrawal of life-sustaining therapy.
- Half of the normothermic patients required a cooling device to avoid fever, so practically will still need early and close monitoring.
- Perhaps the initial mortality benefit to TTM/hypothermia was secondary to the intense monitoring and care delivered, and not specifically the temperature reached.
- This is by far the largest, best designed trial to date, however there is always momentum to maintain the status quo, so it will be interesting to see how this impacts clinical practice and guidelines moving forward.
Take Home:
- It looks like it may be time to cool it (pun intended) with aggressive therapeutic hypothermia. Target normothermia and avoid fever as there is evidence of fever being associated with unfavourable neurological outcomes and no evidence to date of its benefit.
- I think we should be cautious to not interpret this is “do less” for our OHCA patients, but rather to focus on delivering excellent post arrest care with a new temperature target.
- I will still place a temperature probe, but likely hold off on actively cooling normothermic patients in the ED, and discuss with accepting MRP.
- Stay tuned for further studies and to see how guidelines may change to reflect this best level of evidence. The the AAC did just released a statement suggesting pursuing TTM37.8., but AHA ROSC guidelines last came out in 2020, ERC released their guidelines in March 2021 just prior to this study.
- What do you think? Will this change your practice?
References:
- Arrich J et al. Hypothermia for neuroprotection in adults after cardiopulmonary resuscitation. Cochrane Database Syst Rev 2012. :CD004128.
- Bro-Jeppesen J., Hassager C., Wanscher M.et al. Post-hypothermia fever is associated with increased mortality after out-of-hospital cardiac arrest.
Resuscitation. 2013; 84: 1734-1740 - Dankiewicz J, et al. “Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest”. The New England Journal of Medicine. 2021. 384(24):2283-2294. https://www.nejm.org/doi/10.1056/NEJMoa2100591
- Holzer M, et al. “Mild Therapeutic Hypothermia to Improve the Neurologic Outcome After Cardiac Arrest”. The New England Journal of Medicine. 2002. 346(8):549-556.
- Lascarrou J-B. “Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm”. N Engl J Med. 2019. Epub ahead of print:
- Nielsen N, et al. “Target Temperature Management 33°C vs. 36°C after Out-of Hospital Cardiac Arrest”. The New England Journal of Medicine. 2013. 369(23):2197-2206.
- https://www.acc.org/Latest-in-Cardiology/Articles/2021/11/09/13/16/A-Contemporary-Update-on-Targeted-Temperature-Management
https://canadiem.org/targeted-temperature-management-2/
https://emcrit.org/pulmcrit/ttm2/
https://rebelem.com/ttm2-hypothermia-vs-normothermia-for-ohca/
Speak Your Mind
You must be logged in to post a comment.